
The Seventy-sixth World Health Assembly on May 26, 2023, mandated its implementing agency, the World Health Organisation, to extend its traditional medicine agenda until 2025. Accordingly, the WHO’s traditional medicine policy for 2014–2023 was extended by two years until 2025. In addition, the Assembly asked the Director-General to design a new global plan for 2025-2034 and submit it for review to the 78th WHA in 2025.
In this context, there is a need to create an act to establish an indigenous traditional health (paramparik chikitsa) and Knowledge Practice Council and make provisions for promoting, controlling, and regulating indigenous traditional medicine and knowledge. Considering its rich tradition of various achievements in healthcare, Kerala may take the lead in promoting and regulating TCM.
READ I AI in public health: Need to balance innovation with accountability
A traditional medicine agenda
According to the WHO, indigenous traditional medicine is the total knowledge and practices, whether explicable or not, used in diagnosing, preventing, or eliminating physical, mental, and social diseases. This knowledge or practice may rely exclusively on experience and observation handed down orally or in writing from generation to generation. These practices are native to the country in which they are practiced. Most indigenous traditional medicine has been practiced at the primary healthcare level.
The World Health Assembly applauded Member States’ efforts to assess the potential of traditional and complementary medicine (TCM) using a robust evidence-based methodology. Additionally, it acknowledged the importance, diversity, and comprehensiveness of local communities and Indigenous Peoples’ cultural traditions.
The WHA resolution emphasised the significance of WHO’s function in providing technical assistance for incorporating evidence-based T&CM into national health systems and services and supporting the regulation of T&CM practices, products, and practitioners.
Under the 2014-2023 strategy, WHO supports countries that wish to develop a proactive policy towards this important yet often neglected and expanding part of healthcare. WHO’s strategic policy and technical support enable countries to harness the potential of T&CM in contributing to health, well-being, and people-centered healthcare.
Since 2014, WHO has encouraged member countries to build the knowledge base for the active management of T&CM and the appropriate integration, regulation, and supervision of evidence-based, safe, and quality T&CM into national health systems and services. According to the WHO global report on Traditional and Complementary Medicine (2019), national frameworks and infrastructure for traditional and complementary medicine have improved significantly.
Ninety-eight countries reported having a national policy on traditional and complementary medicine, 107 Member States have a national office for traditional and complementary medicine, and 75 Member States have a national research institute for traditional and complementary medicine that is either fully or partially funded by the government. The number of countries with a legal and regulatory framework for traditional and complementary medicine increased from 79 in 2012 to 109 in 2018 and continues to rise (WHO, 2022).
Encouraged by the WHO 2014-2023 strategy, research on traditional and complementary medicine has been conducted globally, including during the COVID-19 pandemic. The WHO International Clinical Trials Registry Platform listed 4,778 traditional medicine-related clinical trials, including 165 trials restricted to COVID-19. In contrast, the WHO COVID-19 database of global literature on coronavirus disease lists 7,516 research articles on traditional medicine (WHO, 2022).
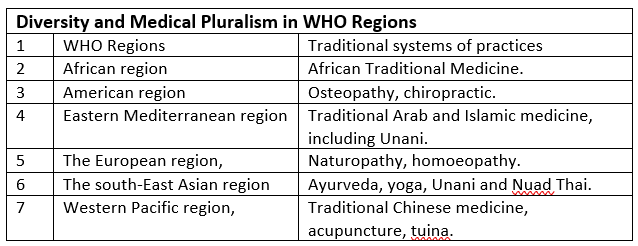
More than one medical system exists in most societies, and patients have faith in diverse medical systems. Medical pluralism (MP) can be defined as the employment of more than one medical system or the use of both conventional and complementary and alternative medicine (CAM) for health and illness.
In India, AYUSH is the acronym for the traditional medical systems practiced in India, such as Ayurveda, Yoga & Naturopathy, Unani, Siddha, and Homeopathy. However, folk medicine and traditional medicine are practiced beyond AYUSH in many parts of the country.
Healthcare systems in India provide an interesting example of medical pluralism. Due to numerous challenges, Indian healthcare practice is pluralistic and unique. Apart from socio-cultural and other gradients, high out-of-pocket (OOPE) expenditure, inadequate institutional facilities, and expensive private healthcare strongly affect the adoption of traditional healthcare practices.
Traditional medicine is an important and often undervalued part of healthcare. Traditional and complementary medicine (TCM) is found in almost every country, and the demand for its services is increasing. Traditional medicine, of proven quality, safety, and efficacy, ensures everyone can access care.
Many governments now recognise the need to develop a cohesive and integrative approach to healthcare that allows governments, healthcare practitioners, and, most importantly, those who use healthcare services to access traditional medicine safely, respectfully, cost-effectively, and effectively (WHO, 2013).
Traditional medicine encompasses a range of sometimes competing health and healing practices, folk beliefs and theories of health and wellness, worldview, religious philosophy, herbal remedies, food, diet, exercise, and treatment specialisations. There is an increasing effort to organise and select elements of philosophy and practice and organise them into what is called traditional medicine.
Various traditions of medicine, such as Zhongyi (traditional Chinese medicine), Ayurveda (Indian traditional medical system), Kampo (Japanese traditional medicine), Hanbang (traditional Korean medicine), Unani, Siddha, and Homeopathy, have been practiced in some areas of the world. They have flourished into orderly-regulated systems of medicine.
The role of traditional and complementary medicine (TCM) in primary healthcare is appreciated by the global health community. As a result, WHO has created a Traditional and Complementary Medicine Unit within the Service Delivery and Safety Department of the World Health Organisation. Recently, with the help of the Government of India, WHO has also established a Global Centre for Traditional Medicine in Jamnagar, Gujarat, India, to promote traditional medicines as a healthcare system.
However, WHO (2013) notes that “inappropriate use of traditional medicines or practices can have negative or dangerous effects” and that “further research is needed to ascertain the efficacy and safety” of such practices and medicinal plants used by traditional medicine systems. As a result, WHO has implemented a nine-year strategy to “support Member States in developing proactive policies and implementing action plans that will strengthen the role traditional medicine plays in keeping populations healthy.”
Traditional and folk medicine are often seen as more accessible, affordable, and acceptable to local populations. They can, therefore, be tools to help achieve universal health coverage. Traditional medicine is commonly used in Africa, Asia, and Latin America.
The main challenges affecting the practice of traditional medicines include stigmatisation due to poor perceptions and attitudes, inadequate efforts to conserve medicinal plants and indigenous knowledge, lack of innovation and modernisation, exploitation of communities that own the knowledge, safety, efficacy, and quality issues, limited access, and irrational use of herbal medicines.
Patterns of traditional and complementary medicine (TCM) use, particularly in primary healthcare, vary among and within countries depending on several factors such as culture, historical significance, and regulations. In some countries, traditional medicine serves as one of the primary sources of healthcare. However, the availability and accessibility of conventional medicine-based health services are generally limited in these countries.
Australia has defined (and regulated) indigenous medicines, traditional Chinese medicines, Ayurveda medicines, homeopathic medicines, and other medicinal products containing herbs, vitamins, and minerals as complementary medicines, which have been incorporated into Australian Medicines Policy.
In 2007-08, the Australian government announced more than $7 million in research grants to strengthen the evidence supporting complementary medicines. Funding of $1.74 million was awarded to establish three National Institute of Complementary Medicine (NICM) Collaborative Centres, and a further $5.3 million was allocated for 13 projects funded by the National Health and Medical Research Council (NHMRC) (Lucas, 2008). The American National Centre for Complementary and Alternative Medicine (NCCAM) has also invested substantial research funds into this area, improving the evidence base.
Around 200 medicinal plant species have been added to the Convention on International Trade in Endangered Species of Wild Flora and Fauna (CITES). However, over two-thirds of the 50,000 medicinal plants in use today are still harvested from the wild, and 4,000–10,000 of them may now be endangered (Hamilton, A., 2003). TCM practitioners rely on herbs and medicinal plants from the wild for treatment, which may contribute to biodiversity depletion. However, TCM practitioners are critical stakeholders in any effort for diversity conservation.
There are several critical questions that remain, such as the nature and extent of practice, the identity of practitioners, their training, skills, and skilling needs, quality assurance processes, regulatory mechanisms, and the involvement of patients and other stakeholders in TCM.
The TCM sector also faces current controversies and problems, including unsubstantiated product claims, lack of proper labeling and warnings, product efficacy concerns, the presence of adulterated and substandard products, harm to patients, lack of independent information about treatments and products, and insufficient research and development efforts.
Given the rise in traditional medicine use, it is important to explore options for ensuring its successful integration into a framework for public health. Additionally, there is a need to develop a policy response to indigenous, traditional, and complementary medicine (TCM) and knowledge in alignment with WHO’s Traditional Medicine Strategy.
Dr Joe Thomas is Global Public Health Chair at Sustainable Policy Solutions Foundation, a policy think tank based in New Delhi. He is also Professor of Public Health at Institute of Health and Management, Victoria, Australia. Opinions expressed in this article are personal.


