
The Union Budget 2023-24 presented by Finance minister Nirmala Sitharaman has allotted Rs 89,155 crore, or 1.98% of the country’s GDP, for healthcare. The outlay is 3.43% higher than the actual expenditure of Rs 86200 crore incurred last year. The increase is insignificant and insufficient considering the state of India’s health infrastructure. India continues to rank among countries with the lowest public health spending. The National Health Policy announced in 2017 had called for the allocation of 2.5-3% of the GDP for healthcare.
Of the total allocation, Rs 86,175 crore is earmarked for the health department and Rs 3,200 crore is for medical research (ICMR). Approximately half of the health department’s budget comes from the National Health Mission which saw a 1.2% increase in allocation from the previous year. Permission has been granted to establish centers for excellence in medical research and to step up collaboration with private institutions.
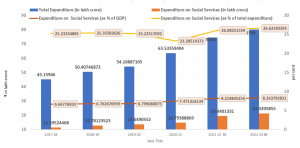
India: Social services expenditure
The AYUSH sector, which includes Ayurveda, Homeopathy, and Unani, has seen a 19.6% increase in outlay. The emphasis is on conducting international development work, generating scientific evidence, and advancing these branches of medicine. Despite reducing financial support to the rural sector, the budget makes no mention of the primary health sector, relied upon by a majority of Indian population.
READ I Budget 2023: The shove to push the Indian economy
Four projects have been prioritised in the health sector:
Elimination of sickle cell disease by 2047
Sickle cell disease is a genetic condition that affects one in every 86 tribal births. In the coming years, 7 crore tribal people under the age of 40 will undergo screening for the disease. The Union government will cover 60% of the cost, while the states are responsible for the remaining funding. However, without proper counseling, privacy, and follow-up care, screening may result in stigma, neglect, and isolation, making it difficult to eliminate the inherited condition.
An example is filariasis disease which was announced as a target for elimination in 2017 despite being a non-genetic communicable disease, and Kala Aznar which was announced as a target in 2020. Both still remain public health concerns. The extension of the target period for their elimination should be a learning experience.
Research in the field of pharmaceuticals
The Budget for the pharmaceutical industry has been increased from Rs 100 crore to Rs 1,250 crore, but the majority of new drug innovations occur in the West. The delay in their availability in India is due to pending patent laws. Currently, India imports most of the raw materials for pharmaceutical manufacturing, known as active pharmaceutical ingredients (APIs), from foreign countries with no domestic price control.
Last year’s figures show that India’s imports were to the tune of Rs 35,000 crore while exports were of Rs 33,000 crore. Despite the Atma Nirbhar Bharat initiative, 41% of medical equipment are still imported, with half of it coming from China. It would be beneficial to establish multidisciplinary courses in the country to develop and produce medical devices.
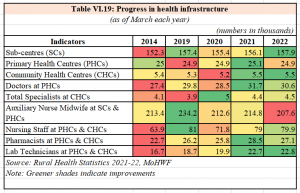
157 nursing schools
In all, 157 medical colleges were established after 2014 and now nursing colleges will also be launched in these institutions. The World Health Organisation recommends a ratio of three nurses per 1,000 people, but India currently has 1.7 nurses per 1,000 people. It is important to not only increase the number of nursing seats, but also retain these professionals within the country. Despite the recent increase in medical college seats, there remains a shortage of specialist doctors with 70% of positions unfilled in community health centers.
Promoting medical research
Encouraging medical research through collaboration between the public and private sectors is being prioritised. To achieve this, the Indian Council of Medical Research (ICMR) will work in partnership with the private sector. One example of such collaboration is the development of the Covid-19 vaccine by Bharat Biotech.
Public health related schemes
The budget has cut funding for non-communicable disease control programmes to Rs 289 crore from last year’s outlay of Rs 500 crore, despite the increase in non-communicable diseases such as diabetes, hypertension, and cancer in the country. This programme also includes national programme for the aged. The social security pension amount for senior citizens and widows has remained unchanged.
The fund for tobacco control programme also falls under this head. At the same time, the tax on cigarettes has been raised by 16% and is being referred to as the National Calamity Duty.
The increase in funding for the Ayushman Bharat health insurance scheme from Rs 6,412 crore to Rs 7,200 crore is insufficient. As of January 4, 4.3 crore individuals have undergone hospital treatment under the scheme. The allocation for the scheme which provides for a maximum cover of Rs 5 lakh for hospital expenditure to over 40 crore people is grossly insufficient. Additionally, several states are currently facing financial difficulties to reimburse the claim backlog.
In 2021, the finance minister had announced an allocation of Rs 35,000 crore for Covid-19 vaccinations. According to the budget document, Rs 220 crore doses of the vaccine were distributed for free to 102 crore individuals in the country. However, the programme finds no mention in this year’s budget. It is also silent on post-Covid treatment for chronic conditions. Rs 133 crore has been allocated for the Digital Health Mission to modernise the health sector.
Health-related and social spending
The largest poverty alleviation programme in the country, the MGNREGA, has seen a 33% cut in outlay. The allocation has been cut from Rs 89,400 crore to Rs 60,000 crore. Economic affairs secretary TV Senath later said that this is because individuals are finding employment in other sectors. He explained that the decrease in demand for the programme is due to economic growth in rural areas.
There has been a 3% cut in the food subsidy budget which has dropped to Rs 28,000 crore from Rs 197,300 crore. The government has clarified that this is due to a decrease in the number of eligible individuals in need of subsidy. There has been a 10% fall in the number of people who require assistance. The fertilizer subsidy has also been cut by 1.5%.
The budget for the school mid-day meal programme has been cut from Rs 12,800 crore to Rs 11,600 crore. The budget for adolescent girls’ nutrition programme remains unchanged at about Rs 20,000 crore. The funds for Anganwadi centers, school lunches, and women and child welfare have been reduced by 40% compared with the outlay for 2014. There have been NFHS reports from the government indicating an increase in malnutrition among women and children in various states of India in recent years.
The national action plan for mechanical sanitation ecosystem (Namaste) has allocated Rs 100 crore to implement fully automated sewage management, which will prevent human scavenging, direct physical exposure to sewage and reduce the number of fatalities caused by manhole accidents in the country. The funding for the Swachh Bharat scheme aimed at eliminating open defecation has been raised from Rs 66,000 crore to Rs 77,000 crore. This allocation will provide toilets to economically disadvantaged households. Last year, the scheme benefitted around 12 crore households.
The Jal Jeevan Mission has received a 27% increase in funding for its Jal Jeevan scheme which looks to provide a minimum of 55 liters of drinking water per day to each household. With this increase, over 9 crore rural homes will have access to tap water.
The health budget, which has both positive and negative aspects, prioritises the well-being of the middle class rather than the neediest, reflecting the belief that economic development through the central government’s policies will result in improved social health outcomes.
(Dr Jayakrishnan T is Professor & HOD, Department of Community Medicine. KMCT Medical College, Calicut. Dr Vidya Kuniyil is Research Assistant, University of Pittsburgh, USA.)

