
By KR Antony
Can we be instrumental in transforming the lives and health of ordinary people — those who are marginalised whose children are working in brick kilns instead of attending schools, whose babies are severely malnourished? To achieve that goal, we need systemic changes to promote healthy living, nutritious food, safe water, sanitation, prevent diseases, deliver good healthcare services and reduce disease impact.
Couple of years back, I was on a panel discussion on the tragedy of infant deaths in hospitals of Gorakhpur, Farrukhabad, Jharkhand and Raipur. The panellists debated whether it is due to lack of oxygen or lack of medical care. They differed on whether it is due to lack of resources or poor governance. All of them were quick to fix the blame on the political party in power. The ruling government, in turn, fixes accountability on a doctor or medical superintendent of the hospital and close the file. Health system failure is barely discussed after mishaps.
The coronavirus disease taught us many lessons. The pandemic was like an MRI of the public health system. It exposed the vulnerabilities and fragility. The public health system was getting dismembered due to several years of neglect in funding, staffing, infrastructure and technology upgradation. But it also proved the relevance and essentiality of a robust public health system. The nation needs it with an immediate upgrade because it is the only option for the poor and the marginalised.
READ I Can Tamil Nadu government create a South Indian Miracle?
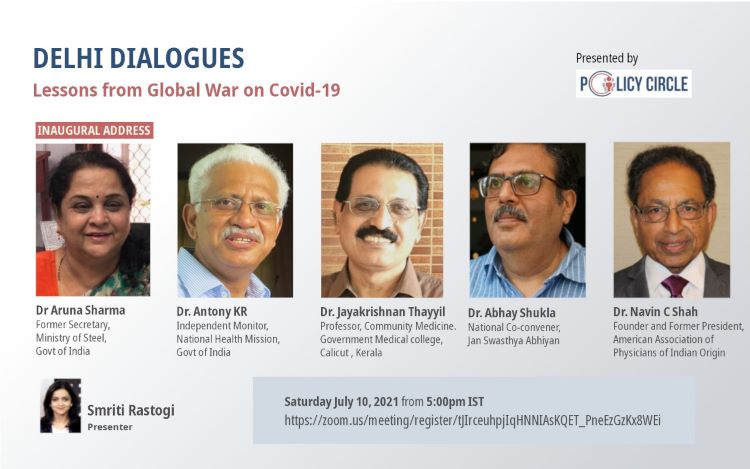
Click on the link to register for this meeting: https://zoom.us/meeting/register/tJIrceuhpjIqHNNIAsKQET_PneEzGzKx8WEi
What are the corrective steps and rehabilitation measures needed for the ailing public health system? We need to reaffirm that health is a basic human right as guaranteed under the constitutional entitlement of Right to Life. But it must be a justiciable right, which it has not become so far. A welfare state should own up the responsibility to provide basic health services, not abdicate this to the private sector or entrust insurance sector to manage it. The private sector is so heterogenous and scattered and its concentration is in urban areas. During this pandemic, private sector displayed a lack of standardisation, medical anarchy and uncontrolled exploitative pricing.
Three fundamental questions on public health system
- Whose health care are we talking about? It is the healthcare for all with equity more than equality, with a concern for the poor, neglected, voiceless and marginalised.
- Who will do it in a democratic, socialist republic? Of course, in a welfare state, it has to be the government, for the people and by the people. We cannot expect the private sector to do it.
- Who should bear the cost? The government of the people from the taxes paid by them, not by the insurance agency.
Globally governments are encouraged to go beyond the primary healthcare as envisaged during the Alma Ata conference to achieve universal health coverage. UHC is a critical component for amelioration of poverty, reducing social inequities and for sustainable development. India is also striving for all these through sustainable development goals or SDGs. Universal health coverage cannot be achieved by roping in private sector and relying on Insurance packages.
Universal health coverage aims at a three-dimensional expansion of health coverage.
- Improving access to people: Wider coverage of beneficiaries in remote locations, forest areas, submerged marshy cut off habitations, islands with increased frequency of services.
- Improving the range of services: Expanding package of services and choice, like a cafeteria menu under modern medicine and AYUSH systems, ranges of services from immunisation, family planning to specialist and intensive care, correction of congenital heart diseases to cochlear implant.
- Improving quality of services: Technological advancement in diagnosis and treatment and accreditation of universal and national standards. There is an overarching goal of improving client satisfaction and stake holder participation and community empowerment.
READ I Covid-19 learnings: Citizens responsible for consequences of their choices
Cost of public health system
UHC requires a financing system to protect people from financial hardship and being pushed into poverty due to healthcare costs. In a democratic country financing health care must be from a “pooled resource” mainly from the tax funds. It cannot be left to the vagaries of market forces or to the insurance sector where enrolment is poor, whether mandatory or voluntary. The expenses are poorly reimbursed and the claim settlement ratio leaves much to be desired.
Health expenditure by government is very low. Proportion of GDP for health budget in percentage was 1.4 % in 2009-10, 1.2 in 2013-14, 1.15 in 2015-16, 1.18 in 2016-17 and 1.3% in 2018-19. Per capita health expenditure varies in states. UP was only Rs 790 per annum compared with the national average of Rs.1538. Low investment in business cannot have big turnover and good profits. Poor spending gives poor returns.
Globally, healthcare expenditure to GDP ratio is 5.99%. Immediate allocation of 3% of the GDP for health sector in India and thereafter incremental increase to reach 6% is what we need. We expected an allocation of around Rs 80,000 crore for health this year, which did not come through. A chunk of 55-60,000 crore should have been allocated for National Health Mission.
READ I The Model Tenancy Act 2020: Towards a maintainable, inclusive rental market
Poverty burden and out-of-pocket expenses
India was moving towards the status of a middle-income country like Brazil, Mexico and South Africa. But the gap between the rich and the poor within the country is widening. Even during the Covid-19 lockdown, 10 Billionaires made enormous profit when overall GDP of the country shrank. India still has a poverty burden with 22% of the world’s poor living in India.
The poor are carrying the challenging double burden of communicable as well as non-communicable diseases. When health expenditure of the government is low, then the cost of that healthcare will be shifted to personal out of pocket expenditure. Because of poverty, 20% of all ailments go untreated (NSSO estimates) unless debilitating, most tend to self-treat, ignore and delay availing of treatment or resort to the locally available cheaper rural medical practitioners and quacks.
Under the prevailing conditions of widening gap between the need and availability of health services, the National Rural Health Mission was launched in 2005. Improving access of rural people, especially poor women and children, to equitable, affordable, accountable and effective primary healthcare was its goal.
The NRHM had a vision of (i) decentralisation for district management of health, (ii) participatory bottoms-up planning, (iii) quality assurance in services and client satisfaction, (iv) inter-sectoral convergence, and (v) defined time-bound goals and reporting publicly the progress on these goals. The key principles followed had a paradigm shift from (i) distrust to trust, (ii) inflexibility to flexibility, (iii) centralized to decentralised action, (iv) funds, functions, functionaries for service, and (v) building capacities at all levels.
The decentralised district plans had widened the scope of addressing local health problems and often required more funds than the centrally driven plans needed. When more funds are demanded, the Union government must ensure an efficient state and district-level health system in place to manage those higher budgetary allocation in a meaningful manner. It must assist states in improving their public health systems with a two- pronged strategy of improving management efficiency and ensuring transparency in transactions.
National level management experts (not political appointed advisors) can be deployed for capacity building in states. A national cadre of public health like the IAS may be constituted. Similarly, there could be a separate state-level public health cadre like that of Tamil Nadu can be built up.
Improving the fund absorptive capacity of NHM
The experience from NRHM was that it needs a stronger professional project management team at district and state levels. Currently around 2,75,000 contractual workers, as consultants and technical hands like paediaticians, obstetricians, anesthetists, business managers, chartered accountants, statisticians, data analysts, surveillance officers and epidemiologists, physiotherapists, counselors, and laboratory technicians.
An army of around 900,000 women, as part-time voluntary workers named ASHAs are seen deployed from the Upper Subhansri district in China border villages in Arunachal Pradesh down to Kanyakumari district of Tamil Nadu and Mizoram to Raan of Kutch. Voluntary is a highly exploitative arrangement to overcome requirements under the prevailing labor laws. ASHAs were the back bone of entire surveillance activity in the community, contact tracing, getting suspects tested, quarantine of the family members and isolation of clinically asymptomatic positives and reverse quarantine of the vulnerable and elderly during the pandemic.
The potential of their utility after simple training is unimaginable as demonstrated by the mitanins in Chhattisgarh, starting from nutrition and immunisation advice, to distribution of ORS, blister packets for tuberculosis and leprosy patients, use of pregnancy kits and rapid diagnostic kits for malaria and use of mucus sucker and Ambu bags for newborn resuscitation. If ASHAs are inevitable as intermediary between the health officials and the local community, we need to accept that reality and pay them the right wages. Charge it to the increased NHM allocation as a meaningful expenditure.
The additional NHM staff proved essential to run the project activities, adding value to programme implementation. The extra staff was the corner stone for transforming health services as a mission instead of a departmental activity. That quality improvement led to the client satisfaction and increased utilisation of services by the public health system. Utilization of government hospitals and health centres improved substantially. If they are inevitable to run the health programme, make them regular employees and pay them just from the extra funds from the NHM.
Another way of improving the utilisation of health sector funds is to think of designing a five-year project plan with annual fund allocation in 5 tranches. Make state planning cycle for 5 years, and not annual. Currently, there is an annual project implementation plan-PIP-development, which is laborious and a time consuming. What are the disadvantages of the annual cycle?
The whole process of reworking on annual planning and budgeting starts from December, submission of the draft plan in January followed by an annual budget allocation made by April. During the February-March period, the whole administrative machinery is busy closing annual account by end March. Initial tranche of funds reaches by June, insufficient to embark upon big budget activities like constructions. So, there is only a small implementation window of 6-8 months, from September to February after release of major funds.
Rigorous work planning will be undertaken only once in 5 years. Broad strategies to achieve general objectives and goals are agreed upon. Phasing of annual financial allocation of the project cycle are spelled out with specific tasks, quantified out puts and expected results. This gives flexibility of continuing long- term activities and carryover of funds at state and district levels.
Submission of expenditure statements and settling accounts with utilisation certificates must become an ongoing process or quarterly affair till end of project cycle. Funds must be earmarked from the beginning of the accounting year for payment of salaries, electricity, water supply, waste disposal, telephones and communication, regular consumables and supplies like oxygen, and essential maintenance.
Universalisation of free drug and diagnostics
Though health is a state subject, there must be full resource allocation for drugs and diagnostics from national government, like any other national programme. Burden of malaria and tuberculosis in a few states must be seen as a national direct responsibility to control rather than leaving it to the state to manage from their share of overall central funds. Jan Oushadi and PMJAY rightly makes provision for this.
In a WHO collaborated study by SHRC on the availability and pricing of essential medicines for children, 50 items surveyed for the first time in the country in Chhattisgarh showed low availability of 17% and a markup price for retailers more than 376%.
Bulk procurement of generic essential medicine through transparent e-tendering was the answer like the model of TNMSC — Tamil Nadu Medical Services Corporation. Six states — Andhra Pradesh, Bihar, Chhattisgarh, Kerala, Rajasthan and Karnataka — have followed the TNMSC example. Delhi, Gujarat and Himachal Pradesh have a central procurement agency.
Tamil Nadu model of procurement and supply of medicines, equipment and consumables must be enforced in all states with poor governance and system failure. Outsourcing or rate-contract based purchase of diagnostics from private sector should give way for an inhouse provision. Insurance-based purchase of secondary and tertiary healthcare from private sector can continue with very stringent oversight and guard against misuse and exploitation till such time the public health system takes over.
Health and wellness centres: HWCs have come up all over the country as a newly branded face of the National Health Mission. It is a mini hospital with 24×7 hours service availability of medical consultation, investigations and dispensing of medicines or provision of first aid and emergency care. A retrained nurse, pharmacist or sector supervisor acts as community health officer along with ANM and ASHA team. Its impact among rural masses is impressive.
Application of information technology and e-governance: This is to eliminate massive corruption in health department and prevent diversion of NHM funds to unintended purposes. It will make the whole governance fair and transparent. It strikes at the root of corruption. We need to practise web-based advertisement of vacant and new posts, recruitment including test and selection interview, appointment and transfer of health staff, for award of contracts for civil works and intake of human resource. Electronic payment of bills and invoices helps tracking of undue delay in payment of cheques with provision for satisfactory reasons for rejection or modification of claim bills.
Human Resource Policy: Now let us discuss how to get health staff to health institutions located in remote areas. Instead of asking why there are no doctors and nurses staying in such difficult areas ask the question why in spite of such constraints and difficulties some doctors and nurses stick on. We asked this as part of a research question in Bastar division of southern Chhattisgarh. It was because they are from the same ethnic back ground or happened to get familiarised with the same geographic and sociocultural milieu due to their parent’s posting or working there. Secondly their own core values and work culture imbibed from their upbringing.
Thirdly their professional interests of treating ill and healing the sick is met there, irrespective of rural or urban location. So, who should be getting to medical schools as future doctors for such areas? A regional recruit of candidates under service bond of 10 years to be trained as doctors or nurses will be most beneficial to the public health system. I have come across one ANM who carries her loaded vaccine carrier and registers climb down 2 hours the slope to a village in Pathalkot under Tamia block in Chindwara district. After the immunisation session, she climbs back this hill for 3 hours with the same load and she does it meticulously without any appreciation.
What makes her do that so sincerely? It is because she has a commitment to her own community known to her and she derives satisfaction in serving her own people. That substantiates the rationale for selection of local candidates with minimum qualification for training to be posted in those districts. Another important aspect is making ANM and GNM posts a district cadre so that they are not posted out too far elsewhere in the state. A tenth class passed tribal girl of Ganiari in Bilaspur district could be trained as echocardiographic technician by a visiting cardiologist of AIIMS New Delhi and deployed in JSS hospital successfully.
In many states there is a lack of a fair non-discriminatory transfer and promotion policy. Whimsical transfers and postings by different authorities at different times demotivate doctors. Staff who have already completed dedicated service for a long time get stuck in the periphery. How to prevent this? As an innovation in Chhattisgarh, we first categorised the location of PHCs into most difficult, difficult and ordinary category. Forest and Naxalite infected areas with difficult road access, poor connectivity for communication etc were some of the criteria for difficult areas.
There could be a three layer of placement circles for doctors. The outer most layer is for a 5-7 years of postings in PHCs and rural dispensaries which may be made compulsory for all new graduates entering the government service. Once they finish a minimum of five years in the outer most layer, they must be shifted to the middle layer which is for posting in the sub district towns with CHC and FRU hospitals. Once they finish 5-10 years of service in the middle circle, they should be brought to the inner most circle of postings in district headquarters and major urban areas.
Once a candidate finished the minimum requirement in a circle, she/he should move to the next layer towards the centre and never to be shunted back to the periphery again. The principles of postings will be always from the periphery to middle and innermost circle and never in the reverse direction. There will be no direct posting of MBBS level to the Specialist Leave Vacancy at District hospitals and Sub-district major towns. Similarly, there will be no post-graduate qualified specialist recruited first posted to PHC-level in the outermost circle.
Community participation and ownership
It is a must for public health system to survive amid commercial competition from mushrooming private sector and to deliver good services. For rejuvenation of a weakened and corrupt public health system, it must rely on ownership by the public and user involvement. Rogi Kalyan Samithis and hospital management committees need to be expanded with representation of user groups and community watchdogs, rather than just one MLA or MP representing people. These user groups and community watchdogs can facilitate social audit of major activities undertaken by health institutions as part of community monitoring.
Strong community ownership has resulted in successful running of palliative care in Kerala. Kerala also showed the utility of investing in social capital of 45,000 extra registered volunteers and 45.4 lakh women entrepreneurs at grass roots called Kudumbashree mission in 290,723 neighborhood groups for Covid-19 control activities. This is in addition to 21,682 elected ward members of 978 village GP and 65 municipal/ corporation councils taking local leadership and working with 26310 ASHA workers and 33,115 Anganwadi workers. It was a large army ready to go the extra mile.
Universal health coverage to universal healthcare
Universal health coverage is what we were discussing so far. India needs to progress from merely expanding universal health coverage to ensuring universal healthcare. What is the difference between the two? Universal healthcare includes various social determinants of health like safe water, sanitation, nutrition, food security, primary education, livelihood, community empowerment, gender and social equity. In the interest of the citizens, we should promote universal healthcare. Then the health ministry has to be serious and proactive for convergence with allied sectors and need to build up its capacity for inter-sectoral coordination.
Comprehensive healthcare is beyond the therapeutic service and scope of the ministry of health and family welfare. For this, we need increased budgetary allocation for determinants of health outcomes like, nutrition, water, sanitation and education sectors. There must be a concomitant increase in the allocation for education, ICDS, food security and livelihood.
Ensuring safe drinking water in all seasons and sanitation coverage to eliminate indiscriminate open defecation must be viewed as a priority investment for the progress of the country. Women carrying pots and buckets of water more than one kilometre distance is seen during summers and in drought prone areas. The three pot figure women carrying a pot of water on the head, baby on the side of chest and another unborn baby inside her abdomen is a familiar sight in many parts of the country.
The amount of calorie diversification in the third trimester of pregnancy for heavy workload is at the cost of intrauterine growth retardation, low birth weight baby and poor neonatal survival. Regularity of Public Distribution System with availability of full component of cereals, pulses and oils will go a long way in improvement of food security and nutrition at household level.
Similarly, a good school enrolment drive followed by satisfactory retention rate and ensuring joyful teaching with minimum levels of learning by the pupils will have very good health outcomes in a decade to follow. Conversely, children who were in school and now out of school, minding cattle and goat on the pastures in many villages is a silent tragedy.
Studies have shown that IMR levels of 120 per thousand reduces to 90 with 4 years of primary schooling and another reduction to 70 with another 4 years of middle school and further IMR reduction to 50 per thousand upon completion of school final by girls. It is heartening to see adolescent girls on cycles going to school, because it is a sure sign of future empowerment and better survival of children and mothers. Former Andhra Pradesh CM Chandra Babu Naidu’s visionary scheme that gave cycles to all girls in high schools heralded a new era of development in the state.
Wealthy cities may not be healthy cities as Mumbai, Delhi, Pune, Hyderabad and Kolkata proved during this pandemic. Weak public health system in cities can make not only the life of urban poor miserable, but also dangerous to others. A large part of urban poor are migrant labourers who are builders of the economy. But they are least enumerated, accounted for and planned for. Provision of basic services — water, sanitation and clean night shelter or temporary dwellings is what we owe them.
Multi-use community centers are needed during cyclones, floods, earthquakes and pandemics for relocation, relief camps, quarantine, community meetings and social events.
- Immediate post-pandemic plans for every district
- Accept and regularise telemedicine as a regular modality for health promotion activities, follow up of NCD, mental illness, and palliative treatment.
- Enforcement of Clinical Establishment Act, regulation of private sector for quality service, pricing and transparency.
- Set up a regional virology research labs and additional vaccine production units in every state.
- Start or facilitate one or two medical oxygen factories in every state with requisite tankers for immediate supply of LMO to hospitals.
- Every state to have centres for communicable disease control. They should take charge in case of an epidemic.
- Allocation of more funds to LSGs for planning, delivery and monitoring of health services under them, including disease outbreak control.
- In every district hospital, establish liquid medical oxygen generation plants of 150 tonne production capacity. Also set up 50 bed isolation wards out of which at least 10 beds should be ICU beds with minimum five ventilator beds.
Along with the vaccination coverage, the government must implement these steps to ensure that we are better prepared for the third wave of the pandemic.
(Dr KR Antony is a public health consultant based in Kochi. He is also independent monitor, National Health Mission.)

