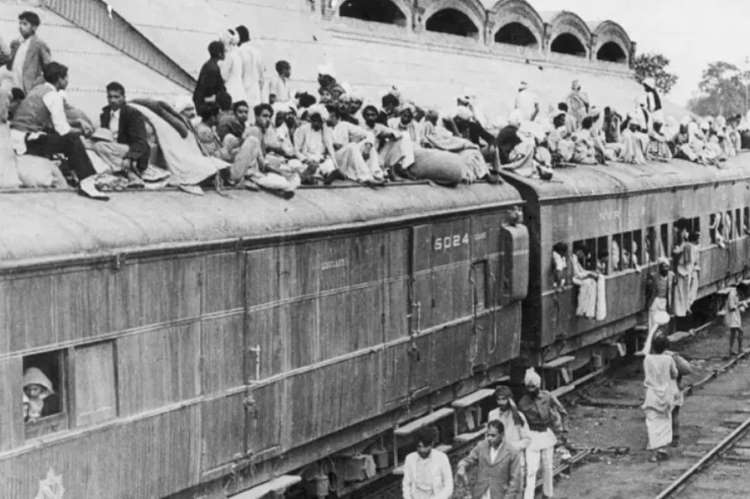
During the Partition, more than fourteen million people were displaced and became refugees, while two million died or went missing, making it one of the most tragic events in history. The partition of the Indian Subcontinent had a profound adverse impact on population, demographics, agriculture, industries, trade, connectivity, logistics, and many other sectors of the economy.
The partition of India in 1947 exacerbated the fragility of the country’s primary healthcare system. The challenging economic situation and communal clashes led to an acute shortage of healthcare professionals and equipment, making it difficult to prevent and control diseases. The sudden mental trauma affected individuals and the collective health of the population, resulting in a calamitous situation. Migration and the refugee crisis limited community participation in health promotion, severely impacting public health. Furthermore, the Western world overlooked the partition as a humanitarian crisis, ignoring the millions of casualties on both sides.
READ I Pakistan plans privatisation drive to save ailing economy
Partition – more than a humanitarian crisis
Post-partition, India and Pakistan were formed, resulting in a disproportionate distribution of the population and land. India received 82.55% of the total population and 77.10% of the land, while Pakistan got 17.44% of the population and 22.89% of the land. A major shortage of raw jute and raw cotton in India starved industries due to the transfer of producing land. Additionally, food production, already declining in the aftermath of World War II, dropped from 53 million tonnes per year before the war to 46 million tonnes in 1946. The loss of major parts of Punjab and the entire Sind to Pakistan, prime food grain-producing regions, coupled with India’s high population density, aggravated the food deficit in India, necessitating reliance on food imports.
India’s share in the global economy, which was about 24.5% before British rule in the 1700s, plummeted to only 4.17% by 1950 after the British left. From 1946 to 1948, India’s GDP witnessed a fractional decrease of about 16.36%, plunging the country into poverty and debt. A disturbed economy led to reduced investment in healthcare, further limiting access to already overstressed healthcare services, especially in underserved or rural areas, exacerbating health disparities.
During the partition, the struggling economy led to deteriorating public health. Medical assistance from international agencies like the British Red Cross was insufficient to meet India’s primary healthcare needs. The simultaneous emergence of medical emergencies in refugee camps, coupled with injuries from communal clashes, overwhelmed the country’s healthcare services.
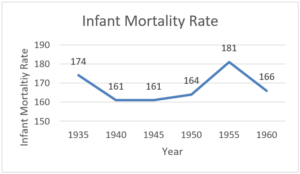
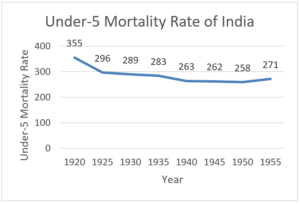
Infants and children under five years equally experienced the brutalities and trauma of the partition. Historical data show a 10.36% increase in the infant mortality rate (IMR) in India post-partition in the 1950s (from 164 per 1000 live births in 1950 to 181 per 1000 live births in 1955). Infant mortality in India was stagnant from 1935–45 and only began declining again in the 1960s. Similarly, under-five mortality, which had been declining from 1920 to 1950, increased by 4.8% between 1950 and 1955 (from 258 to 271 per 1000 live births). Pre-partition levels of under-five mortality were only regained in the 1960s.
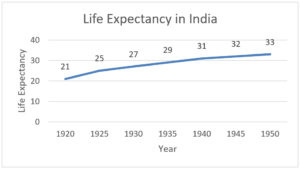
Life expectancy was only 32 years at the time of partition. Although there was a constant increase in life expectancy, data show a deceleration during the post-partition period (1925–25.75 years, 1930–27.98 years, 1935–29.9 years, 1940–31.6 years, 1945–32.7 years, 1950–33.9 years). We can conjecture that without the partition, the declining trend of infant and under-five mortality and the rise in life expectancy would have continued, resulting in economic gains.
Despite such a momentous human loss, our review reveals only twenty-four publications on the subject between January 1947 and December 1951. We conclude that the international scientific community, the United Nations, and aid organisations did not significantly address this catastrophic event. Our review suggests the crucial role of the international scientific and research community as vigilant fact-finders to unearth the facets of mass human tragedy and its long-term consequences, thereby awakening global consciousness and ensuring help and aid flows when most needed.
In contrast, the ongoing Israel-Palestine war in Gaza demonstrates the tremendous influence of the scientific community, civil society, and the press. This conflict has captivated global public attention and mobilised direct action by civil society. As a result of this mass awakening, the UN Security Council (UNSC) in 2024 passed a historic resolution calling for an immediate ceasefire in Gaza with overwhelming support. This step is historic as the UNSC has passed 342 resolutions mentioning ceasefire since its inception, with only two landmark occasions directly calling for a ceasefire in the Israel-Palestine conflict, in 2009 and 2024.
The post-World War era witnessed a gradual increase in concern by the scientific community on the health aspects of victim populations, reflected in the extensive coverage of contemporary crises such as the Palestine-Israel conflict, the Myanmar refugee crisis, the Yemen war, and the Ukraine-Russia war. The recent UNSC resolution marks a watershed moment, highlighting the power of the pen, media, and civil society in mobilising collective action for a ceasefire and alleviation of human suffering.
However, silent sufferings around the world continue to impact large populations and impede the attainment of Sustainable Development Goals. United Nations data indicate that about 7.8 million people have died in battle-related deaths between 1989 and 2022. The lack of centralised data on humans and the health effects of various conflicts often limits comprehensive quantitative and qualitative analysis. The effects of man-made conflicts on human health need greater attention from the scientific community, which, through a multi-dimensional stakeholder analysis, should work towards increasing the visibility of sufferings faced by vulnerable populations. Highlighting the health impact of conflicts should bring these issues to the forefront of discussions and evoke relief and corrective actions. The recent UNSC ceasefire resolution is an excellent model to emulate in all such conflicts.
(Dr Rakesh Sarwal is a civil servant. Dr Tuba Tanveer is a public health professional based in New Delhi. Views expressed are personal.)
