
Cervical cancer, often described as a silent killer, remains overshadowed as the world grapples with medical emergencies like pandemics. The disease affects women of various ages, socioeconomic statuses, and geographical regions. Cervical cancer impacts the lower part of the uterus, the cervix, and typically shows no symptoms in the early stages. However, women should be vigilant about symptoms like abnormal vaginal bleeding, pelvic pain, and unusual discharge, which should prompt them to seek a comprehensive medical examination and diagnosis.
To reduce their and their children’s risk of Human HPV infection and associated cancers, women need to be informed about the HPV vaccine. The relative survival rate for early-detected cancer is 91%, compared with 60% for late diagnoses. Early detection significantly enhances the chances of a full recovery and effective treatment. Women are encouraged to prioritise their reproductive health and to access healthcare services, including screenings, vaccinations, and necessary treatments, by raising awareness about cervical cancer.
READ I Kerala’s heat waves a sign of climate change’s unequal impact
Women can choose their preferred method of cervical cancer screening by understanding the differences between HPV testing and Pap smears. HPV tests identify high-risk HPV strains that can lead to cervical cancer, while Pap smears detect abnormal cell changes in the cervix. A tailored screening strategy may be beneficial based on their age, personal preferences, and risk factors. The fifth round of the National Family Health Survey (NFHS-5), conducted from 2019 to 2021, included a specific question on cervical cancer screenings, asking women, “Have you ever undergone a screening test for cervical cancer?” Only 1.2% of the 765,805 women aged 15 to 49 who responded had undergone a cervical cancer screening.
Government’s commitment to women’s health
In the 2024 Interim Budget, the government announced a focus on vaccinating girls between the ages of 9 and 14 against cervical cancer. This programme reflects the commitment to addressing women’s health issues, particularly those related to cervical cancer, and preventive healthcare. By targeting this age group, the government seeks to protect individuals from HPV before potential exposure through sexual activity, emphasising the importance of preventing cervical cancer and how vaccinations can reduce the incidence of the disease. For this purpose, the interim Budget 2024–2025 allocated Rs 87,656.90 crore to the department of health and family welfare. The HPV vaccine is currently available in private hospitals at a cost of up to Rs 4,000 per dose.
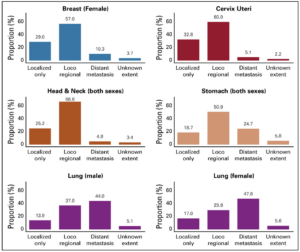
Relative proportion (%) of cancer patients
Sexual behaviors linked to an increased risk of cervical cancer include having multiple sexual partners, early marriage, and poor genital hygiene. Additionally, cofactors such as smoking and prolonged use of contraceptives increase susceptibility to Human Papillomavirus (HPV) infection, the primary risk factor for cervical cancer.
Cervical cancer ranked as the fourth most common cancer globally and the fourth leading cause of cancer-related deaths among women in 2020, with an estimated 604,127 new cases and 341,831 deaths. It is the second most common cancer among women in India, with 123,907 new cases and the second largest cause of cancer-related deaths, with 77,348 deaths expected in 2020. India accounts for 21% of new cases and 23% of deaths worldwide from cervical cancer, recently surpassing China in the number of new cases and fatalities.
Investing in women’s well-being
Investing in women’s health enables women to take control of their health and well-being. Women with access to resources, education, and healthcare services are better equipped to make informed decisions about their health and to advocate for their needs within their communities. Prioritising their health facilitates early detection and prevention of diseases such as breast and cervical cancer and reproductive issues. Better health outcomes and reduced healthcare costs result from this focus. Achieving gender equality requires investment in women’s well-being. Education, reproductive rights, and access to healthcare services empower women and advance their equality in society.
The well-being of women is closely linked to the well-being of families and communities. Healthy mothers are more likely to raise healthy children and contribute positively to their communities’ socioeconomic status. Enhancing the well-being of women offers substantial benefits for the wider community. In their roles as caregivers and health advocates within their families and communities, women often play pivotal roles.
Reducing incidence of cervical cancer
Recognising the specific challenges faced by women, especially those from lower socioeconomic backgrounds and rural areas, has led to a paradigm shift in the government’s approach to preventing cervical cancer. Girls in rural areas are often married off at a young age, increasing their vulnerability to HPV infections. Early childbirth also heightens the risk of this cancer.
By focusing vaccine efforts on girls in this age bracket, the government shifts from reactive to preventive healthcare. This proactive approach lowers healthcare costs and improves health outcomes by recognising the importance of disease prevention. Another aspect of the paradigm shift is the emphasis on raising awareness and educating communities and women about cervical cancer. By increasing knowledge about the HPV vaccine, regular screenings, and the signs and symptoms of cervical cancer, women are better equipped to take charge of their health and make informed decisions.
A major barrier to preventing cervical cancer is the public’s lack of awareness about the importance of routine screenings, HPV vaccination, and early detection. Many people may overlook the early symptoms of cervical cancer, delaying diagnosis and treatment. Disparities in access can result from the inability to afford preventive interventions such as vaccinations and screenings. Social stigma associated with HPV and sexual activity may prevent individuals from discussing or seeking information about preventive care.
The need for action is clear. The advancements in cervical cancer prevention, from vaccination programmes to public awareness campaigns, call on all citizens to assume the roles of community advocates, policy reformers, and global champions for women’s health.
(Mitanshi Shah is student, and Dr Barun Kumar Thakur is Associate Professor at the department of economics at FLAME University, Pune.)

